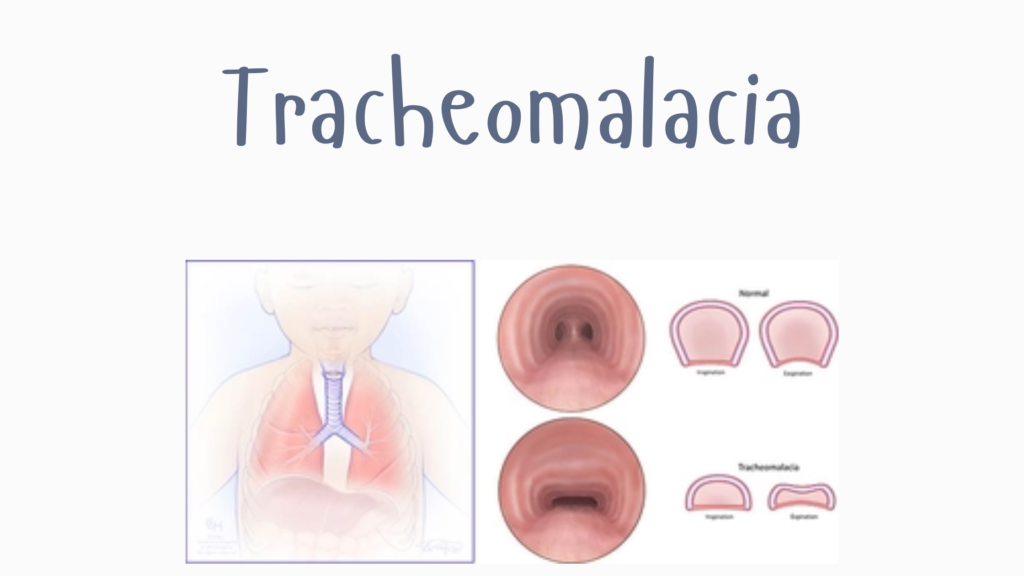
Tracheomalacia is a condition where the tracheal walls are weak or floppy, causing the trachea to collapse—especially during exhalation, coughing, or crying. This leads to airway obstruction, noisy breathing, and other respiratory symptoms.
🧬 What Happens in Tracheomalacia?
The cartilage rings in the trachea, which normally keep it open, are either underdeveloped (congenital) or become weakened (acquired). This causes:
- Airway collapse during expiration (when pressure inside the chest is high)
- Airflow limitation, especially when increased breathing effort is needed
🧒🧑 Types of Tracheomalacia
1. Congenital Tracheomalacia
- Present at birth
- May occur alone or with other anomalies (e.g., tracheoesophageal fistula, esophageal atresia)
- Often improves with age as cartilage stiffens
2. Acquired Tracheomalacia
- Occurs later due to:
- Prolonged intubation or tracheostomy
- Infections
- Chronic inflammation (e.g., from GERD, tracheitis)
- External compression (e.g., tumors, vascular rings)
- Relapsing polychondritis (autoimmune)
📋 Symptoms
- Noisy breathing (especially during exhalation)
- Stridor or wheezing that doesn’t respond to asthma meds
- Chronic cough
- Frequent respiratory infections
- Difficulty breathing, especially when crying, coughing, or feeding (in infants)
- Cyanosis (blue skin/lips) in severe cases
🧪 Diagnosis
- Flexible bronchoscopy – gold standard; visualizes dynamic collapse of airway
- CT scan with dynamic expiratory imaging – shows narrowing of tracheal lumen
- Fluoroscopy – for dynamic airway assessment
- Pulmonary function tests (in older children/adults)
💊 Treatment Options
✅ Mild Cases (especially congenital):
- Often improve with age
- Supportive care: humidified air, chest physiotherapy, careful monitoring
- Manage GERD if present
🩺 Moderate to Severe Cases:
- CPAP or BiPAP – keeps airway open during breathing
- Tracheostomy – for airway support (in severe cases)
- Aortopexy – surgical procedure to relieve airway compression
- Tracheal stenting – used in selected adult cases (risks include infection, granulation tissue)
🛡️ Prognosis
- Congenital tracheomalacia often improves by 18–24 months
- Acquired cases depend on cause and response to treatment
- Long-term issues possible if severe or associated with other conditions
🧠 Important Distinctions
| Condition | Primary Feature | Treatment Focus |
|---|---|---|
| Tracheomalacia | Collapsing trachea (soft cartilage) | Airway support, surgery if needed |
| Asthma | Bronchial inflammation/narrowing | Inhalers, bronchodilators |
| Laryngomalacia | Floppy laryngeal tissue | Often resolves spontaneously |