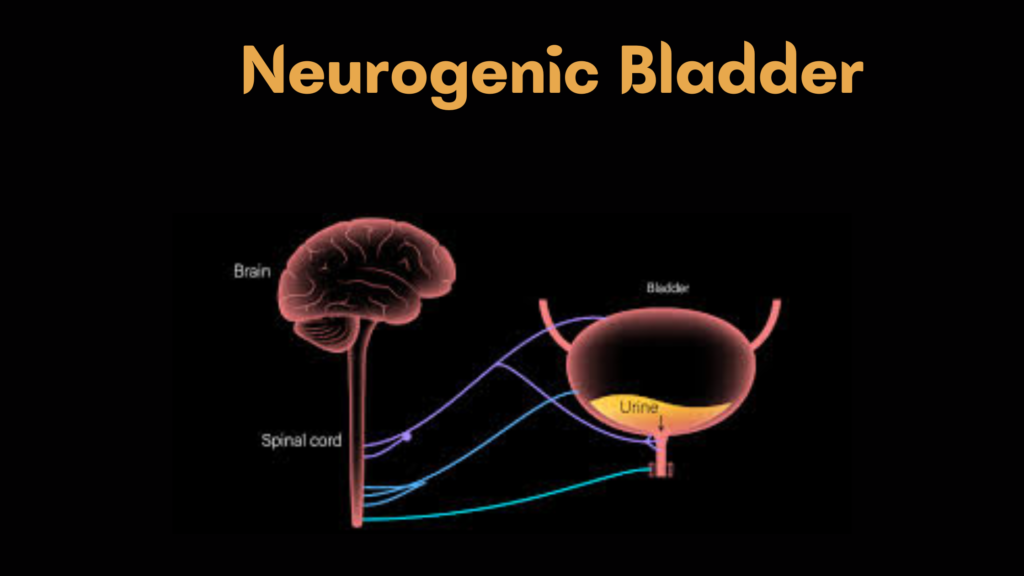
Neurogenic Bladder Neurogenic bladder is a dysfunction of the urinary bladder caused by problems in the nervous system —specifically the nerves that control bladder storage and emptying. It can result in urinary incontinence , retention , infection , or kidney damage if untreated.
🧠 Causes of Neurogenic Bladder Cause Example Conditions Spinal cord injury Trauma, tumor, surgery Neurological diseases Multiple sclerosis, Parkinson’s disease, stroke Congenital defects Spina bifida (myelomeningocele), cerebral palsy Peripheral nerve damage Diabetes, pelvic surgery, chronic alcoholism
📋 Types of Neurogenic Bladder Type Description Overactive (spastic) Frequent, uncontrolled contractions → urge incontinence Underactive (flaccid) Poor or absent bladder contraction → urinary retention Detrusor-sphincter dyssynergia (DSD) Sphincter and bladder contract at the same time → obstruction
⚠️ Symptoms Urinary urgency and frequency Incontinence (urge or overflow) Urinary retention Hesitancy or weak stream Recurrent urinary tract infections Hydronephrosis or kidney damage (in severe cases) 🧪 Diagnosis History & Physical Exam Focus on neurologic findings and voiding pattern Urinalysis and Culture Bladder Ultrasound Assess post-void residual (PVR) urine volume Urodynamic Testing Evaluates bladder pressure, capacity, detrusor function, and sphincter coordination Cystoscopy Rule out anatomic causes or assess mucosa Imaging (e.g., MRI, CT, spine X-ray) To evaluate underlying neurologic causes or upper tract damage 🩺 Treatment Tailored to the type and severity of dysfunction.
🔹 Behavioral & Non-Pharmacologic Timed voiding / bladder training Pelvic floor exercises Intermittent self-catheterization (CIC) 🔹 Medications Purpose Medications Reduce bladder overactivity Anticholinergics (e.g., oxybutynin, solifenacin), β3-agonists (mirabegron) Improve bladder emptying Cholinergic agents (e.g., bethanechol) – rarely effective Reduce sphincter tone Alpha-blockers (e.g., tamsulosin) in men
🔹 Procedural & Surgical Botox injections into detrusor (for overactive bladder)Sphincterotomy or urethral stent (for DSD)Bladder augmentation (for small, high-pressure bladders)Urinary diversion (in severe, refractory cases)🛡️ Goals of Management Protect kidney function Achieve safe bladder emptying Prevent infections and complications Improve quality of life 📈 Complications (if untreated) Recurrent UTIs Bladder stones Vesicoureteral reflux (VUR) Hydronephrosis Renal failure