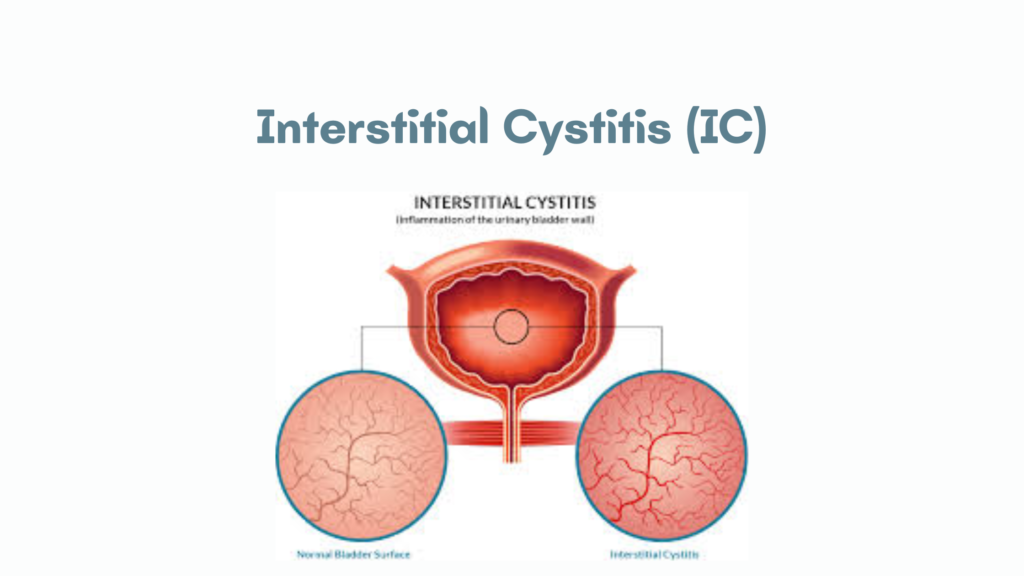
Interstitial Cystitis (IC)
Also called Bladder Pain Syndrome (BPS), interstitial cystitis is a chronic bladder condition characterized by pelvic pain, urinary urgency, frequency, and discomfort, without an identifiable infection or other obvious cause.
🔍 Overview
- Idiopathic and chronic
- More common in women (female-to-male ratio ~5:1)
- Symptoms can range from mild to severe and can greatly affect quality of life
⚠️ Symptoms
- Chronic pelvic or suprapubic pain (worsened with bladder filling)
- Urgency and frequency (often urinating >8 times/day, including at night)
- Painful urination
- Dyspareunia (painful intercourse)
- No infection found on urine cultures
🧪 Diagnosis
- Diagnosis of exclusion: Rule out UTIs, bladder cancer, stones, and other causes
- Urinalysis and urine culture: Usually normal
- Cystoscopy with hydrodistention (under anesthesia):
- May reveal glomerulations (petechial hemorrhages)
- Hunner’s ulcers (classic lesions in some cases)
- Potassium sensitivity test (less commonly used)
🩺 Pathophysiology (Theories)
- Defective bladder epithelial lining → increased permeability (“leaky bladder”)
- Mast cell activation and inflammation
- Neural hypersensitivity
🩹 Treatment
Multimodal and individualized:
1. Lifestyle and Behavioral
- Avoid bladder irritants (caffeine, alcohol, spicy foods)
- Stress reduction
- Bladder training
2. Oral Medications
- Pentosan polysulfate sodium (Elmiron®) – only FDA-approved oral drug
- Amitriptyline or other tricyclic antidepressants (pain relief)
- Antihistamines (e.g., hydroxyzine)
- Analgesics for pain
3. Bladder Instillations
- Dimethyl sulfoxide (DMSO)
- Heparin, lidocaine, or other compounds
4. Physical Therapy
- Pelvic floor therapy for muscle spasm or dysfunction
5. Surgery
- Reserved for severe refractory cases
📈 Prognosis
- Chronic condition with variable course
- Many patients experience symptom improvement with treatment but no definitive cure
- Quality of life can be significantly affected, requiring multidisciplinary management