Crohn’s disease is a chronic, relapsing inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract from the mouth to the anus . It causes patchy, transmural (full-thickness) inflammation , which may lead to strictures, fistulas, and nutrient malabsorption.
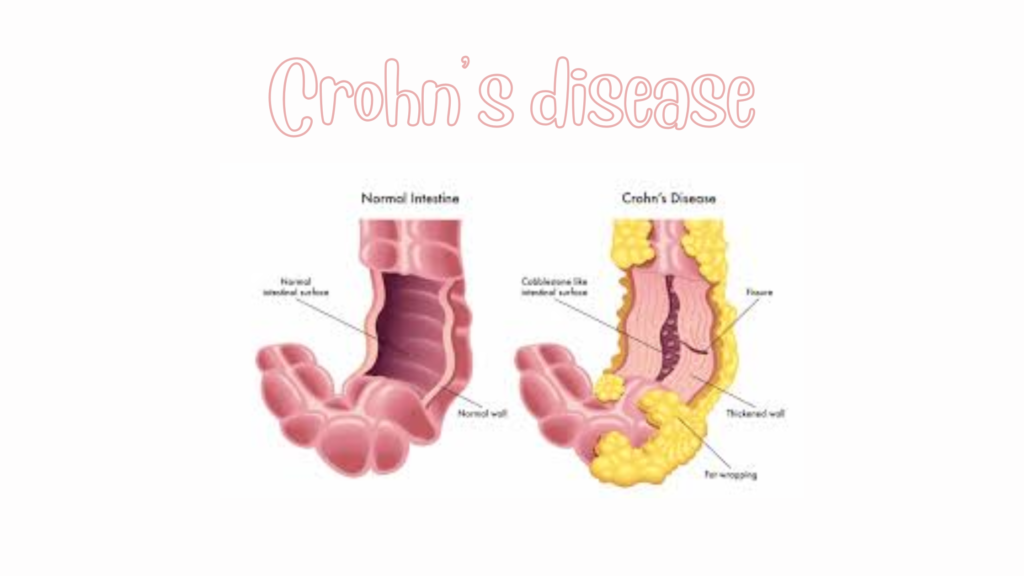
🧬 Pathophysiology Believed to result from immune dysregulation , genetic susceptibility (e.g., NOD2 gene ), and environmental triggers. Causes non-continuous (“skip”) lesions with transmural inflammation , meaning all layers of the bowel wall are affected. Leads to ulceration, fibrosis, and fistula formation . ⚠️ Common Locations Terminal ileum and proximal colon most often involvedCan affect entire GI tract (mouth to anus) Perianal disease common (fistulas, abscesses, skin tags)😖 Symptoms Gastrointestinal Systemic/Extraintestinal Chronic diarrhea (± blood) Fatigue Abdominal pain (crampy)Weight loss Fever Low-grade fever Mouth ulcers Arthritis , uveitis , skin rashes (e.g., erythema nodosum)Rectal bleeding (less common than UC)Anemia , malnutritionPerianal disease Fistulas, abscesses, fissures
🧪 Diagnosis ✅ 1. Colonoscopy with Biopsy Gold standard for diagnosis Skip lesions , cobblestone appearance , deep ulcers Histology: granulomas (non-caseating, in ~30% of cases) ✅ 2. Imaging MR enterography or CT enterography : evaluates small bowel involvement, strictures, abscesses, fistulasCapsule endoscopy : for small bowel mucosal visualization✅ 3. Lab Tests CRP , ESR elevatedFecal calprotectin : marker of gut inflammationCBC : anemia, leukocytosisVitamin and mineral levels (B12, iron, folate, D)🔍 Crohn’s vs Ulcerative Colitis Feature Crohn’s Disease Ulcerative Colitis Distribution Mouth to anus, skip lesions Continuous from rectum upward Wall involvement Transmural (full thickness)Mucosal and submucosal only Granulomas Often present Absent Rectal involvement Variable Always involved Perianal disease Common Rare Surgery Not curative May be curative (colectomy)
💊 Treatment 🔹 Induction (for flare-ups) Mild to Moderate Moderate to Severe Budesonide (ileal disease) Systemic corticosteroids 5-ASA (less effective in Crohn’s) Biologics (anti-TNF, anti-integrins, IL-12/23 blockers) Antibiotics (e.g., metronidazole for perianal disease) Immunomodulators (azathioprine, methotrexate)
🔹 Maintenance Therapy Immunomodulators : Azathioprine, 6-MP, methotrexateBiologics :Anti-TNF : infliximab, adalimumabAnti-integrin : vedolizumabAnti-IL-12/23 : ustekinumabJAK inhibitors : newer options (e.g., upadacitinib)🔹 Surgical Management Not curative (unlike UC) Indicated for:Obstruction Fistulas/abscesses Strictures Failure of medical therapy 📉 Complications GI Complications Systemic/Extraintestinal Strictures Anemia Fistulas (enteroenteric, perianal) Osteoporosis Malabsorption/nutrient deficiency Joint, eye, and skin diseases Increased cancer risk (colon) Growth delay in children Abscesses, perforation Liver disease (PSC less common)
🛡️ Lifestyle & Monitoring Smoking cessation (smoking worsens Crohn’s)Nutritional support (may need B12, iron, D, calcium) Colonoscopy every 1–2 years if colonic involvement >8 years Vaccination: avoid live vaccines if on immunosuppressants