Celiac disease is a chronic autoimmune disorder triggered by the ingestion of gluten—a protein found in wheat, barley, and rye—in genetically susceptible individuals. It causes inflammation and damage to the small intestinal lining, leading to malabsorption and a wide range of symptoms.
🧬 Pathophysiology
- Gluten is ingested → broken down into gliadin.
- In people with HLA-DQ2 or HLA-DQ8 genes, gliadin triggers an immune response.
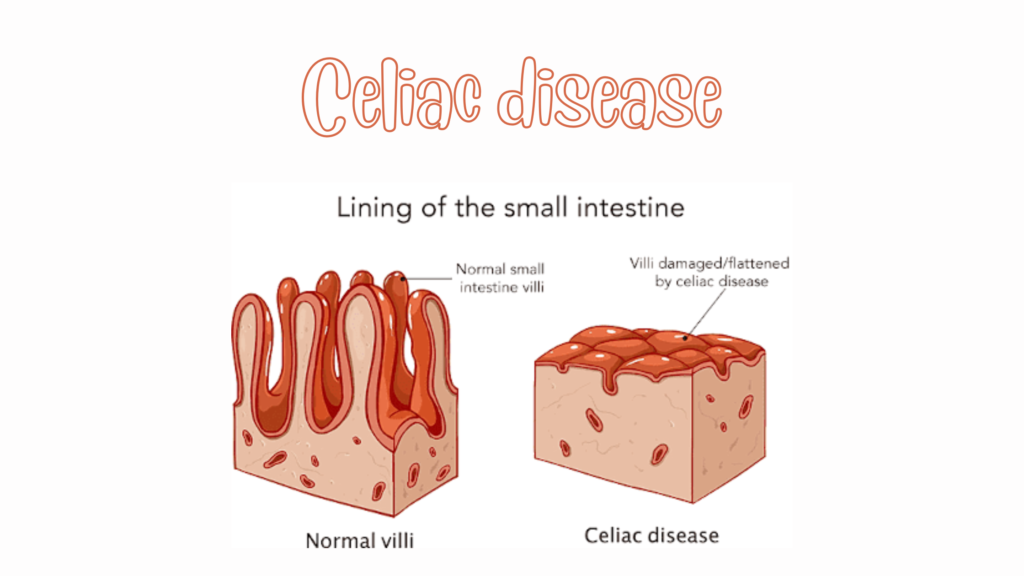
- This leads to immune-mediated destruction of the small intestinal villi (villous atrophy).
- Result: malabsorption of nutrients, including iron, calcium, folate, and fat-soluble vitamins.
⚠️ Risk Factors
- Family history of celiac disease
- Other autoimmune conditions (e.g., type 1 diabetes, autoimmune thyroiditis)
- Genetic markers: HLA-DQ2 (~95%) or HLA-DQ8 (~5%)
- Down syndrome, Turner syndrome
😖 Symptoms
Celiac disease can be classical (GI-related) or non-classical (extra-intestinal):
🔹 Gastrointestinal Symptoms
- Chronic diarrhea or constipation
- Abdominal pain, bloating, gas
- Weight loss
- Fatigue
- Nausea, vomiting
- Foul-smelling, bulky stools (steatorrhea)
🔹 Non-Gastrointestinal Symptoms
- Iron deficiency anemia (often unresponsive to oral iron)
- Osteoporosis or osteopenia
- Dermatitis herpetiformis (itchy, blistering skin rash)
- Neurological issues: headaches, brain fog, peripheral neuropathy
- Infertility or miscarriage
- Delayed growth or puberty in children
🧪 Diagnosis
✅ 1. Serologic Testing (while patient is still eating gluten)
- Anti-tissue transglutaminase IgA (tTG-IgA) – most sensitive and specific
- Total serum IgA – to check for IgA deficiency (common in celiac)
- If IgA deficient: test tTG-IgG or deamidated gliadin peptide IgG
✅ 2. Endoscopic Biopsy of the Duodenum
- Confirms diagnosis
- Shows villous atrophy, crypt hyperplasia, and increased intraepithelial lymphocytes
🧬 3. Genetic Testing (HLA-DQ2/DQ8)
- Helpful to exclude disease: if both absent, celiac is extremely unlikely
🚫 Gluten-Free Diet (GFD) = Main Treatment
🔹 Strict lifelong avoidance of:
- Wheat (and its derivatives: spelt, durum, semolina)
- Barley
- Rye
- Oats (only if not certified gluten-free due to contamination)
✅ Allowed Foods:
- Rice, corn, quinoa, buckwheat, potatoes
- Fresh fruits and vegetables
- Meat, fish, poultry (unprocessed)
- Gluten-free labeled products
💡 Watch for hidden gluten in:
- Soy sauce
- Salad dressings
- Soups, processed meats
- Medications and supplements
📉 Complications (if untreated)
| Complication | Description |
|---|---|
| Malabsorption | Nutrient deficiencies |
| Osteoporosis | Due to calcium and vitamin D loss |
| Infertility | In both men and women |
| Dermatitis herpetiformis | Chronic blistering skin condition |
| Enteropathy-associated T-cell lymphoma (EATL) | Rare but serious GI cancer |
| Small intestinal adenocarcinoma | Very rare |
🔄 Celiac Disease vs Non-Celiac Gluten Sensitivity vs Wheat Allergy
| Feature | Celiac Disease | NC Gluten Sensitivity | Wheat Allergy |
|---|---|---|---|
| Immune mechanism | Autoimmune | Possibly immune-mediated | IgE-mediated (allergy) |
| Villous atrophy | Yes | No | No |
| Serology (tTG, EMA) | Positive | Negative | Negative |
| Allergy testing | Negative | Negative | Positive |
| Lifelong gluten-free diet | Yes | Often recommended | Avoid wheat only |
🩺 Monitoring and Follow-Up
- Symptoms typically improve in weeks to months after starting GFD
- Repeat tTG-IgA at 6–12 months to monitor adherence
- Repeat biopsy not routinely needed unless symptoms persist
- Monitor for nutrient deficiencies (iron, B12, folate, D, calcium)