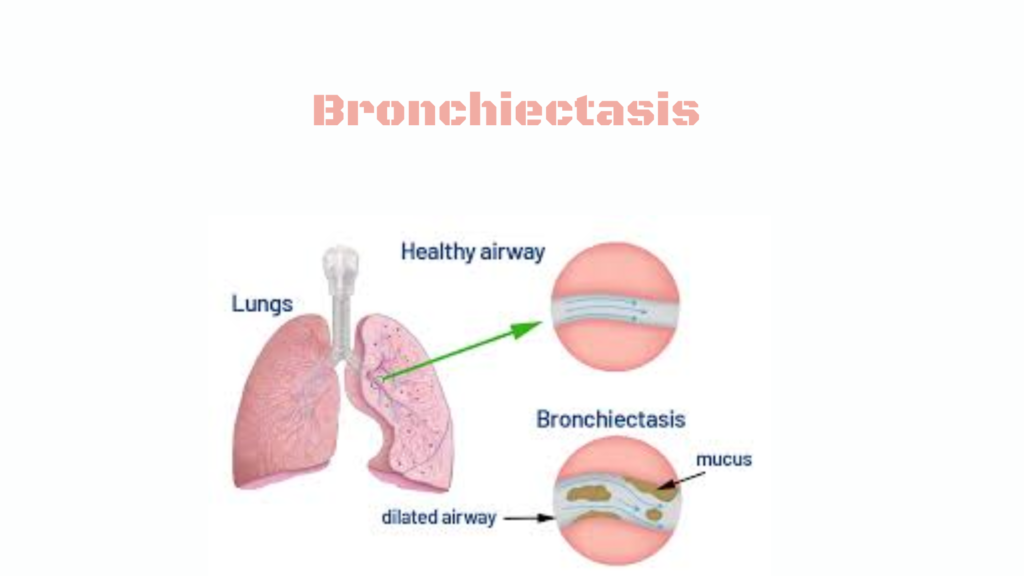
Bronchiectasis is a chronic lung disease where the bronchi (airways) become permanently widened, scarred, and inflamed due to repeated infection or injury. This leads to poor mucus clearance, which causes persistent infection, chronic cough, and airway damage.
🧬 Pathophysiology
- Inflammation and infection → destruction of bronchial wall tissue
- Mucociliary clearance is impaired → mucus builds up
- Trapped mucus becomes a breeding ground for bacteria
- Results in a vicious cycle of infection → inflammation → damage
🚨 Causes of Bronchiectasis
🔹 Post-infectious (most common)
- Severe pneumonia
- Tuberculosis
- Whooping cough
🔹 Genetic / Congenital
- Cystic fibrosis (most common inherited cause)
- Primary ciliary dyskinesia
- Immunodeficiencies (e.g., IgA deficiency)
🔹 Obstructive
- Tumors
- Foreign body aspiration
- Enlarged lymph nodes
🔹 Autoimmune / Inflammatory
- Rheumatoid arthritis
- Inflammatory bowel disease
- Allergic bronchopulmonary aspergillosis (ABPA)
📋 Symptoms
- Chronic productive cough (daily for months or years)
- Thick, purulent sputum
- Recurrent chest infections
- Hemoptysis (coughing up blood)
- Shortness of breath
- Wheezing or crackles on auscultation
- Fatigue and weight loss (in severe cases)
🧪 Diagnosis
🔍 Clinical suspicion
- Persistent cough with sputum
- History of recurrent infections
🧪 Investigations:
- High-resolution CT scan (HRCT) – gold standard
→ Shows “tram-track” appearance or “signet ring” sign - Sputum cultures – identify bacteria (e.g., Pseudomonas, Haemophilus)
- Pulmonary function tests – show obstructive pattern
- Blood tests – for immune deficiencies or autoimmune diseases
- Sweat chloride test / genetic testing – if CF is suspected
💊 Treatment
1. Airway Clearance
- Chest physiotherapy (percussion, postural drainage)
- Oscillatory PEP devices (e.g., Acapella, Flutter)
- Nebulized saline (helps thin mucus)
2. Antibiotics
- Oral or IV antibiotics for infections
- Inhaled antibiotics (e.g., tobramycin) for chronic colonization (esp. Pseudomonas)
- Macrolides (e.g., azithromycin) may help reduce exacerbations
3. Bronchodilators & Steroids
- If coexisting asthma or COPD
- Not standard for isolated bronchiectasis unless indicated
4. Treat underlying cause
- CF, immunodeficiency, ABPA, etc.
5. Surgery
- Rarely needed, but can be considered for:
- Localized disease not responding to treatment
- Frequent bleeding (hemoptysis)
📊 Complications
- Recurrent pneumonias
- Respiratory failure
- Massive hemoptysis
- Pulmonary hypertension (late stage)
🛡️ Prevention & Self-care
- Vaccinations (influenza, pneumococcal)
- Avoid smoking and pollutants
- Practice good hand hygiene
- Regular follow-up and sputum monitoring
🧠 Summary Table
| Feature | Bronchiectasis |
|---|---|
| Cause | Infections, genetic, autoimmune |
| Symptoms | Chronic cough, thick sputum, hemoptysis |
| Diagnosis | HRCT chest |
| Treatment | Airway clearance, antibiotics, address underlying cause |