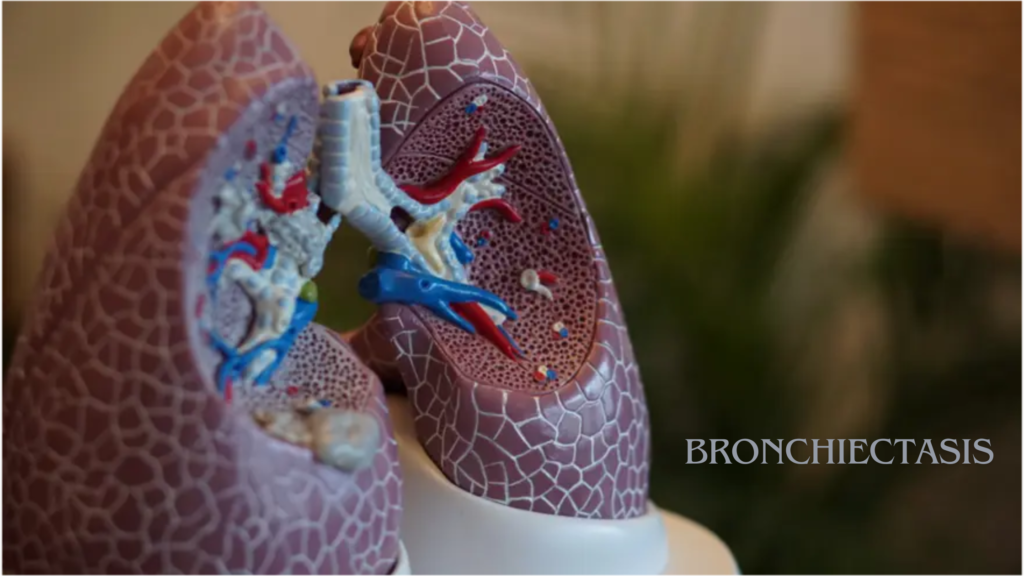
🫁 Bronchiectasis
Bronchiectasis is a chronic lung condition in which the bronchial tubes (airways) become abnormally widened and damaged, leading to a build-up of mucus, recurrent infections, and breathing difficulties.
It is not contagious, but it can get progressively worse over time if not managed properly.
🔍 What Happens in Bronchiectasis?
- Normally, the airways are elastic and lined with small hairs (cilia) to move mucus out.
- In bronchiectasis, the airways lose elasticity, become floppy or scarred, and can’t clear mucus efficiently.
- This leads to a cycle of infection → inflammation → more airway damage.
📋 Common Symptoms
- Chronic, productive cough (lasting months or years)
- Daily production of thick sputum (may be yellow or green)
- Shortness of breath, especially with activity
- Wheezing
- Chest pain or tightness
- Frequent lung infections
- Fatigue
- Clubbing (swelling of the fingertips) in advanced cases
🧪 Causes
Bronchiectasis can be caused by many conditions, including:
Post-infectious
- Severe or repeated lung infections (e.g., pneumonia, tuberculosis, whooping cough)
Underlying Medical Conditions
- Cystic fibrosis (CF) – the most common genetic cause
- Primary ciliary dyskinesia
- Immunodeficiency (weakened immune system)
- Allergic bronchopulmonary aspergillosis (ABPA)
- Autoimmune diseases (e.g., rheumatoid arthritis, Sjögren’s syndrome)
Other
- Airway obstruction (e.g., tumor or foreign body)
- Inhalation of toxic gases or chronic aspiration
🩺 Diagnosis
- High-resolution CT scan: The gold standard for diagnosing bronchiectasis (shows dilated airways).
- Chest X-ray (less sensitive)
- Sputum culture (to identify bacteria)
- Lung function tests (spirometry)
- Blood tests (to find underlying causes)
💊 Treatment and Management
Although bronchiectasis cannot be cured, it can be managed to reduce symptoms and prevent progression:
Airway Clearance
- Chest physiotherapy (percussion, postural drainage)
- Mucus-thinning agents (e.g., hypertonic saline, nebulized medications)
- Inhalers (bronchodilators)
Medications
- Antibiotics (oral, inhaled, or IV for infections)
- Anti-inflammatory medications (in some cases)
- Vaccinations (flu, pneumonia, pertussis)
Other Support
- Pulmonary rehabilitation
- Oxygen therapy (for advanced cases)
- Surgery (rarely needed; for localized disease)
🔄 Prognosis
- Many people live well with proper management.
- Without treatment, bronchiectasis can lead to respiratory failure or heart problems (like cor pulmonale).