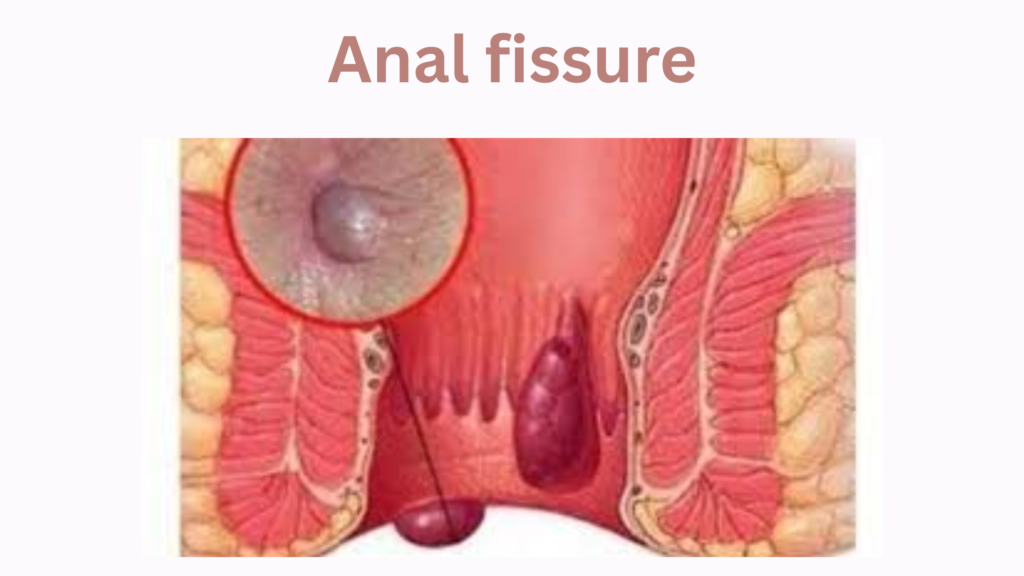
An anal fissure is a small tear or ulcer in the lining of the anal canal, typically caused by trauma during bowel movements. It leads to pain, bleeding, and sometimes spasm of the anal sphincter.
🧬 Pathophysiology
- Most fissures occur in the posterior midline of the anus.
- Less commonly, they occur anteriorly.
- Chronic fissures may have exposed internal sphincter fibers, a sentinel pile (skin tag), and/or a hypertrophied anal papilla.
⚠️ Causes & Risk Factors
- Hard stools (constipation)
- Straining during bowel movements
- Chronic diarrhea
- Anal intercourse
- Childbirth
- Inflammatory bowel disease (e.g., Crohn’s disease – especially for lateral fissures)
😖 Symptoms
- Sharp, severe pain during and after defecation (can last minutes to hours)
- Bright red blood on toilet paper or surface of stool
- Visible tear at the anal verge (on exam)
- Spasm of the internal anal sphincter (exacerbates pain)
🧪 Diagnosis
- Usually clinical, based on history and gentle physical exam.
- Visual inspection reveals a linear tear in the anoderm (typically at 6 o’clock in supine position).
- Digital rectal exam and anoscopy often deferred if too painful in acute phase.
- Persistent or atypical fissures (lateral, multiple) may require further evaluation to rule out:
- Crohn’s disease
- HIV
- Syphilis
- Tuberculosis
- Cancer
💊 Treatment
🔹 Conservative (First-line for acute fissures)
- High-fiber diet (20–30g/day)
- Stool softeners (e.g., docusate)
- Sitz baths (warm water soak 10–15 min after BMs, 2–3×/day)
- Topical anesthetics (e.g., lidocaine)
🔹 Medical Therapy for Chronic Fissures
- Topical vasodilators:
- Nitroglycerin 0.2–0.4% ointment (increases blood flow, relaxes sphincter)
- Apply twice daily; common side effect: headache
- Nifedipine or diltiazem cream/gel (fewer side effects than nitroglycerin)
- Nitroglycerin 0.2–0.4% ointment (increases blood flow, relaxes sphincter)
🔹 Botulinum Toxin Injection
- Relaxes internal sphincter
- Alternative for those who fail medical therapy
🩺 Surgical Treatment (for refractory cases)
- Lateral internal sphincterotomy (gold standard)
- Divides a portion of the internal sphincter to reduce spasm and promote healing
- High success rate (>90%), but small risk of incontinence
📉 Prognosis
- Acute fissures: often heal with conservative care in 4–6 weeks
- Chronic fissures: may require medical or surgical intervention
- Recurrence is common if risk factors persist
✅ Prevention
- Avoid constipation and straining
- Maintain adequate hydration
- Eat a fiber-rich diet
- Promptly treat diarrhea or constipation