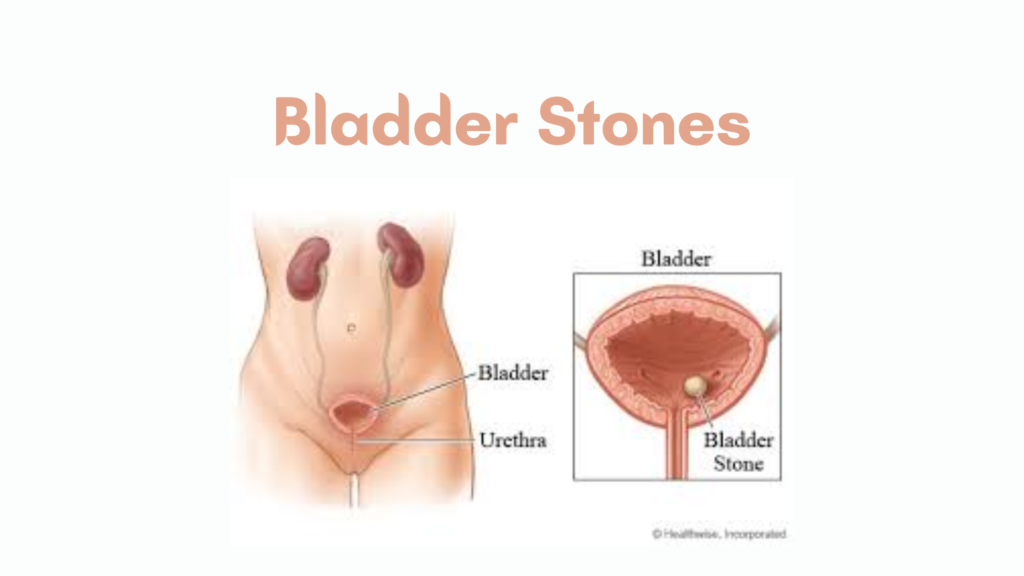
Bladder Stones
(Also called vesical calculi)
Bladder stones are hard mineral deposits that form in the urinary bladder, often due to urinary stasis, infection, or foreign bodies. They are less common than kidney stones but can cause significant urinary symptoms.
🧬 Pathophysiology
Bladder stones typically form when:
- Urine becomes concentrated, leading to crystallization.
- Urinary retention or incomplete emptying allows minerals to accumulate.
- Foreign bodies or devices (e.g., catheters) act as a nidus for stone formation.
⚠️ Common Causes
| Cause | Notes |
|---|---|
| Bladder outlet obstruction | BPH (benign prostatic hyperplasia), urethral stricture |
| Neurogenic bladder | Impaired bladder emptying |
| Chronic infections | Especially with urease-producing bacteria (e.g., Proteus) |
| Foreign bodies | Indwelling catheters, surgical sutures |
| Bladder diverticula | Pouches that retain urine |
| Migration from kidneys | Rare, but possible |
⚠️ Symptoms
- Dysuria (painful urination)
- Urinary frequency or urgency
- Intermittent urine stream or retention
- Hematuria (blood in urine)
- Pelvic pain
- Recurrent UTIs
- May be asymptomatic if small
🧪 Diagnosis
- Urinalysis
- May show hematuria, infection, or crystals
- Imaging
- X-ray (KUB): detects radiopaque stones (e.g., calcium)
- Ultrasound: detects echogenic stones with shadowing
- CT scan (non-contrast): most sensitive for all stone types
- Cystoscopy
- Direct visualization, often used for diagnosis and treatment
🩺 Treatment
🔹 Small Stones (sometimes <5 mm)
- May pass with hydration and bladder flushing
- Observation if asymptomatic and no obstruction
🔹 Most Stones Require Removal
- Endoscopic removal (cystolitholapaxy)
- Most common: stone is crushed and removed via cystoscope
- Done under local, spinal, or general anesthesia
- Open surgery (cystolithotomy)
- For large stones or when endoscopy fails
- Percutaneous techniques
- Minimally invasive alternative in certain cases
🧠 Prevention
- Treat underlying causes:
- Relieve bladder outlet obstruction (e.g., TURP for BPH)
- Remove foreign bodies
- Manage chronic infections
- Encourage adequate hydration
- Regular bladder emptying in patients with neurogenic bladder
📈 Prognosis
- Good if treated early
- Recurrence is possible if the underlying cause isn’t corrected